A melanoma diagnosis, while less common than other skin cancers, is serious. AHN is here to see you through your diagnosis and treatment plan.
What is melanoma?
Melanoma is the most serious type of skin cancer, arising from melanocytes, the cells that produce melanin, the pigment that gives skin its color. Melanoma develops when melanocytes change and start to grow abnormally. These abnormal cells can then spread to other parts of the body through the bloodstream or lymphatic system.
Skin Cancer Center of Excellence
The AHN Melanoma and Skin Cancer Center of Excellence is unlike any other skin cancer center in the area. Our dedicated team of dermatologists, oncologists, oncodermatologists, and medical professionals are all working in tandem to provide the most comprehensive and compassionate care to our patients.
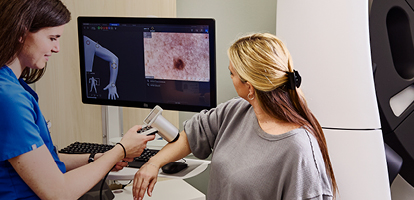
With a team of expert providers and state-of-the-art technology, we’re able to provide comprehensive skin cancer screening, diagnostic services, and specialized care for high-risk patients all in one setting to ensure consistent and thorough care.
Why choose AHN for melanoma treatment?
At the AHN Cancer Institute, you’re never alone. You will find treatment that is:
- Personalized: Our skilled team of dermatologists, oncologists, pathologists, and surgeons work in tandem to offer the latest targeted, minimally invasive surgeries or therapies pinpointed to treat the type of skin cancer you have.
- Patient-centric: Our Navigation Team helps coordinate appointments, answers questions about symptoms and treatment options, and provides logistical support if you need to travel. We help lift the burden of logistics so you can focus on getting better.
- Compassionate: Cancer treatment is a stressful time. Our compassionate team of caregivers is devoted to improving your quality of life, helping you understand treatment options, and keeping you comfortable every step of the way. Our robust support services help bridge some of the gaps that can happen during treatment.
- Collaborative: Your treatment team works together to provide what’s right for you — whether it’s surgery, medical oncology, or radiation therapy.

Quick guide to melanoma
Melanoma symptoms and signs
Melanoma, the most serious type of skin cancer, can be tricky to spot, but early detection is crucial for successful treatment. Doing regular skin checks and having regular preventive care can be a way to spot changes before they become concerning.
Here are some key symptoms to look for when doing skin checks—specifically when looking at changes in moles. You can remember the categories using acronym ABCDE:
- A — Asymmetry: One half of the mole doesn't match the other half.
- B — Border: The edges are irregular, notched, or blurred.
- C — Color: The color is uneven, with shades of brown, black, tan, red, white, or blue.
- D — Diameter: The mole is larger than 6 millimeters (about the size of a pencil eraser).
- E — Evolving: The mole is changing in size, shape, or color.
Other warning signs or concerning symptoms:
- New moles: Any new mole that appears after the age of 30 should be checked by a dermatologist.
- Itching, tenderness, or pain: These symptoms can indicate that a mole is changing or becoming cancerous.
- Bleeding or scabbing: A mole that bleeds or scabs without a clear reason should be examined.
- Unusual texture: A mole that feels rough, firm, or bumpy may be a sign of melanoma.
Melanoma risk factors
Melanoma can spread rapidly. Often, patients with melanoma have many moles and might have a family history of melanoma. Using risk factors and our expertise, we specialize in monitoring high-risk patients to find and detect melanoma early when it’s more easily treated.
If we suspect melanoma, we will perform a biopsy of the affected area. Your care team, made up of highly trained pathologists, oncologists, and dermatologists work to quickly and accurately diagnose suspected melanoma.
Melanoma screening and diagnosis
Early cancer detection saves lives. We offer monthly cancer screenings across Pennsylvania so you can find resources when and where you need. Melanoma is more aggressive, so early detection is essential.
A physical exam
A physician, often a dermatologist, examines your skin to look for suspicious growths. Basal and squamous cell carcinomas tend to look red and flaky. Melanomas are often larger and multi-colored.
While it usually arises on sun-exposed areas, melanoma can present on any part of the skin or body, like under your nail. This is called subungual melanoma. This is a serious type of skin cancer that develops under your nail. It most commonly appears as dark brown or black streaks on your nail. While much less common, acral melanoma is another subtype that affects those with darker skin tones and presents on the skin of palms or soles of the feet.
Talking with your doctor about your risk factors and any new symptoms is critical for detecting the types of melanoma that are found on the skin, eyes, or in mucous membranes.




Mole mapping
This procedure uses full-body photographs of your skin to monitor changes in existing moles and to detect new ones. Physicians use this cutting-edge preventive measure at your annual skin exam. It’s especially helpful for tracking moles for high-risk individuals, such as those with a family history of melanoma.
Biopsy
A small tissue sample is collected to be examined by pathologist who specializes in dermatology. A biopsy can determine if cancer is present. During a biopsy, an anesthetic is given so the sample can be collected comfortably.
Biopsy procedures include:
- Shave biopsy, using a tool similar to a razor
- Punch biopsy, using a circular tool that removes a small section of skin
- Excisional biopsy, using a scalpel to remove an entire lump
Sentinel lymph node mapping
Sentinel lymph node mapping is a surgical technique used to determine if cancer has spread from the primary tumor to nearby lymph nodes.
In a skin cancer diagnosis, specialists use this minimally invasive melanoma diagnostic tool to remove a sentinel node near cancerous tissues. The sample goes to a pathologist who specializes in skin cancer to determine if the node contains cancer cells and if the cancer has spread. Right now, we are using this for melanoma and other aggressive skin cancers including Merkel cell carcinoma. Our researchers are pioneering this technique for squamous cell cancer as well.




Melanoma types
Melanoma has four different types:
- Superficial spreading melanoma: The most common type, often appearing as a flat lesion with irregular borders and varying colors that spreads horizontally. It usually can be found on the torso, legs, or arms.
- Nodular melanoma: A raised, firm, and often darkly pigmented nodule (bump) that accounts for about 15% of melanomas. It can grow quickly and is often found on the torso and head.
- Lentigo maligna melanoma: Making up about 5% of melanomas, this is a slow-growing cancer that typically appears on sun-exposed areas like the face. It appears as a flat, brown or tan lesion with irregular borders, or may have a freckle-like appearance.
- Acral lentiginous melanoma: This type can occur on the palms, soles of the feet, mucus membranes, or under the nails, often appearing as a dark streak or band. It makes up about 5% of melanomas and progresses at varying rates.
Stages of melanoma
The staging of melanoma helps determine the extent of the disease and guides treatment decisions. It’s based on the thickness of the tumor, the spread to nearby lymph nodes, and whether it has metastasized (spread) to distant organs. Your AHN care team is highly skilled in diagnosing melanoma, so your treatment meets your specific needs.
Stage 0 (melanoma in situ)
The cancer is confined to the top layer of skin (epidermis) and has not spread to deeper layers. It’s also known as melanoma in situ or superficial spreading melanoma in situ. It’s considered the earliest stage and has a very high cure rate with surgical removal.
Stage I melanoma
The tumor is less than 1 mm thick and has not spread to lymph nodes. It’s further divided into two different ‘stages based on the tumor thickness: Stage IA (tumor thickness less than 0.75 mm) and Stage IB (tumor thickness 0.75 mm to 1 mm). The prognosis is generally good with surgical removal for both substages.
Stage II melanoma
The tumor is thicker than 1 mm but has not spread to lymph nodes.It's further divided into Stage IIA (tumor thickness 1.01 mm to 2 mm), Stage IIB (tumor thickness 2.01 mm to 4 mm), and Stage IIC (tumor thickness greater than 4 mm). The prognosis is generally good with surgical removal, but the risk of recurrence increases with thicker tumors.
Stage III melanoma
The cancer has spread to nearby lymph nodes.It’s further divided into Stage IIIA (lymph nodes involved but no distant metastasis), Stage IIIB (lymph nodes involved and distant metastasis), and Stage IIIC (lymph nodes involved and distant metastasis).The prognosis is more complex and depends on the extent of lymph node involvement and the presence of distant metastasis.
Stage IV melanoma
The cancer has spread to distant organs, such as the lungs, liver, brain, or bones. It’s considered the most advanced stage and has a poorer prognosis.




Melanoma treatment
Your melanoma treatment options at the AHN Cancer Institute are comprehensive, cutting edge, and include a whole-person approach so your total well-being is considered.
Treatment options include surgery, radiation therapy, chemotherapy, and immunotherapy, but the goal is often to manage symptoms and improve quality of life.
Melanoma is a more aggressive form of skin cancer that can be life-threatening if left untreated. Our pathologists are skilled in melanoma detection. They are adept at staging and tracking its growth. This level of precision helps your team tailor a treatment option just right for you.
Melanoma surgery
Our highly skilled surgeons use the latest techniques and technologies. They collaborate closely with oncologists, dermatologists, and pathologists to determine the best surgical approach for you. Our advanced surgical options include:
- Excisional surgery: We surgically remove cancerous tissue and a very small area of surrounding healthy skin.
- Plastic and reconstructive surgery: This cosmetic surgical procedure helps restore your appearance after an excessive amount of skin or tissue has been removed.
Radiation therapy and medical oncology
If the cancer has spread, we use advanced treatments to stop cancer in its tracks.
Radiation therapy
We deliver high-dose radiation beams directly to a tumor. Targeting only the tumor minimizes your overall radiation exposure. We are also the only radiation oncology network accredited in western Pennsylvania by the American College of Radiology. This accreditation means AHN meets specific guidelines for patient safety, quality control, and efficiency of equipment. You’re receiving the highest-quality treatment available.
Immunotherapy
We may recommend oral immunotherapies for melanoma tumors that are locally aggressive and tumors that have spread to Stage III and beyond the lymph nodes. AHN oncologists are at the forefront of melanoma research and use the newest drug therapies, including new treatments like ipilimumab and pembrolizumab that may help treat and prevent the return of melanoma.
TVEC and TILs treatment
T-VEC is a genetically engineered virus that targets and destroys melanoma cells, while TILs are a patient’s own immune cells that are grown in the lab and infused back into the body to fight melanoma. Both treatments are effective for melanoma and are typically utilized in patients who have failed immunotherapy treatment. T-VEC is more widely available and can be used for both localized and metastatic melanoma, whereas TILs are used for metastatic melanoma and require a more complex inpatient treatment regimen.
Contact us
Call the Hope Line at (412) 578-HOPE (412) 578-4673 to connect with a nurse navigator or schedule an appointment.

